The INSURE strategy
Established benefits of surfactant, while avoiding prolonged MV1*
Early rescue INSURE strategy following nCPAP failure may help avoid the potential for respiratory insufficiency and the need for subsequent MV.1 In several studies, CUROSURF was administered via the early rescue INSURE strategy with a surfactant dosing threshold as low as 0.30.2†
*It is important to note that the INSURE strategy may not be appropriate for all infants. Infants with RDS may vary markedly in the severity of respiratory disease, maturity, and presence of other complications, and thus it is necessary to individualize patient care.
†Dosing threshold ranged between 0.30 and 0.55.2-5
INSURE: INtubation, SURfactant, Rapid Extubation
- Initial intubation in NICU within 1 to 2 hours of birth6
- When respiratory support with a ventilator is likely needed, early surfactant administration and rapid extubation is preferable over prolonged ventilation6
- Extubation should be performed when the infant is stable and at the discretion of the clinician
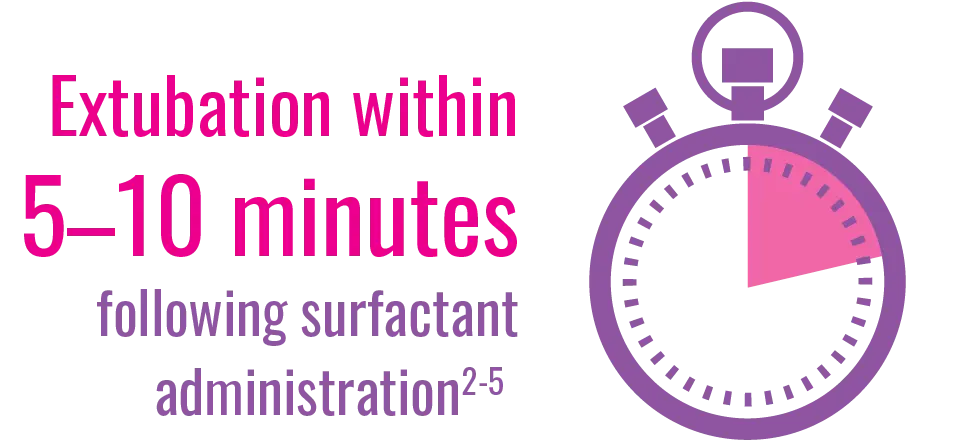
- In some clinical studies, infants treated with CUROSURF using the INSURE strategy were generally extubated within approximately 5 to 10 minutes following surfactant administration2-5
- Rapid extubation after surfactant administration may not be achievable or desirable in the most immature infants, and decisions to extubate should be individualized7